Thymectomy for Myasthenia Gravis and Thymoma
Thymectomy is the removal of the thymus, a gland which is part of the body’s immune system located in front of the heart, behind the breast bone and in between the lungs. It is responsible for fighting against foreign substances, but enlarges in some people and contributes to the development of muscle weakness (myasthenia gravis). Myasthenia gravis can be treated by removing the thymus. This has no effect on the immune system. 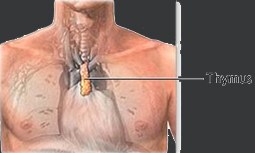
Benefits in removing the thymus reduce the weakness in muscles and help in the full recovery from the illness.
Indication
People who are recommended to undergo this procedure should be under 60 years of age with moderate to severe cases of myasthenia gravis. People with mild muscle weakness may be advised to undergo thymectomy if it affects swallowing and breathing, but not so much with people who have weakness in the eye muscle.
Thymectomy is also advised if a mass is found in the thymus (thymoma).
Procedure
Approaches to this procedure have three different variations:
- Transsternal: Your doctor makes an incision through your breast bone (sternum). If necessary, the fat tissue next to the thymus is also removed. This is the most commonly used approach.
- Transcervical: Your doctor makes a horizontal cut at the lower neck and sometimes even the chest to remove fat near the thymus.
- Videoscopic (VATS): This is a less invasive method that creates small incisions on the chest to introduce a tiny camera and thin, flexible tubes to view and remove the thymus and fatty tissues.
Risks
Complications associated with this procedure include:
- Bleeding
- Infection
- Damage to other organs
- Nerve injury
- Respiratory failure
What to expect
Before performing the procedure, certain protocols need to be accomplished. Your clinical records will be reviewed and you will be ordered to undergo complete physical exam. Certain tests will be ordered such as:
- X-rays
- Blood tests
- Urine tests
- Muscle strength tests
- Breathing tests
The procedure will be discussed with you, giving you surgical options, possible complications and the results.
If you are taking medications, you may be asked to stop or change the dose of the drug. Intake of foods and fluids is restricted 6-8 hours before the surgery.
Recovery
- A ventilator may be required after the surgery. You will be encouraged to do deep breathing and coughing exercise once the equipment is removed to clear the lungs from any accumulation of fluids or mucus.
- One or two chest tubes may be placed to continually drain the fluid.
- Pain killers will be given to control the pain.
- Gradually perform activities from light to heavy until you are fully recovered.

 Multimedia
Multimedia Location and
Location and